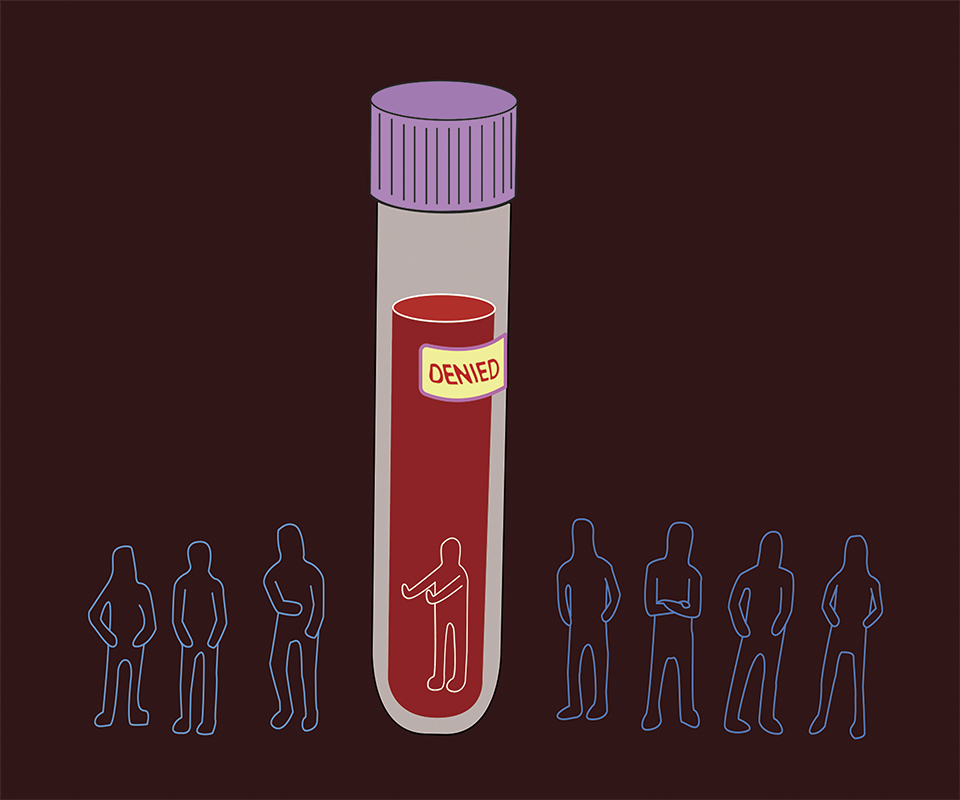
Héma-Québec singles out homosexual and bisexual men.
Héma-Québec held a blood-drive in Concordia’s LB building this past week, but not everyone was allowed to donate.
Héma-Québec’s website provides a list of criteria for who can and cannot donate. The section “men who have sex with men,” stateS that if a man’s “last sexual contact with a man was less than 12 months ago,” he cannot donate blood.
In 2016-17, close to 360,000 people volunteered in Héma-Québec blood drives. Over 316,000 blood products, such as whole blood, plasmas, platelets, and red blood cells were delivered to hospitals. Once blood is donated, it undergoes testing for various viruses, bacterias, and diseases. If anything is detected, the blood sample is destroyed to ensure only healthy blood products are given to hospitals.
In the late 1970s, more than 1,000 people contracted HIV and Hepatitis C from contaminated blood, in Canada. It became clear that the blood screening process at the time was not effective. In order to combat this, the Royal Commission of Inquiry on the Blood System was formed in 1993, and recommended the quality of blood products and the safety of the recipients be of top priority.
Héma-Québec states that the 12-month waiting period was created with the Commission in mind. It considers the fact that gay men are statistically more likely to contract HIV.
According to Statistics Canada, “there were approximately 1,396 new infections in 2014 attributed to the men who have sex with men (MSM) exposure category, representing 54.3 per cent of all new infections.” However, the same source also found females infected with HIV in 2014 made up an estimated 23.2 per cent of all new infections, and the majority of these women contracted the virus through heterosexual contact.
“I think the rule is outdated,” said Akira De Carlos, a health and resource coordinator for Queer Concordia. De Carlos said homosexual and bisexual men find it unfair that they are unable to give blood. “Just statistics-wise, if you’re homosexual, it does not mean that you will necessarily get HIV,” said De Carlos.
AIDS Community Care Montreal (ACCM) “feels that the current blood donation guidelines are discriminatory and unscientific,” said Ren Haskett, education for prevention coordinator for ACCM. “Men who have sex with men are unfairly targeted by the current criteria, regardless of their actual sexual practices and risk level,” added Haskett.
ACCM is the only “English-language community organization that provides services for people living with HIV or Hepatitis C,” said Haskett.
They added that the 12-month deferral period does not reflect the current science behind HIV testing. “A year long deferral period is also not reflective of current science as the window period for the nucleic acid amplification testing used to test blood donations for HIV is only nine days.” These tests look at genetic material to detect bacteria and viruses in the blood, which allows for earlier identification of diseases.
“It’s 2018, health services have changed. Safe-sex education is more available and accessible,” said De Carlos. “Treatments and medical methods have evolved as well.”
There are some changes in the works, according to Haskett: “Héma-Québec and Canadian Blood Services are exploring behaviour-based screenings for all donors.”
The Canadian Blood Services website defines behaviour-based screening as a long-term solution. These screenings would determine potentially high-risk behaviour in a donor based on how many sexual partners they’ve had and their safe sex practices. This way, patients’s safety would still come first, while also limiting the societal impact on specific groups like the LGBTQ+ community.
Graphic by @spooky_soda.