Concordia and McGill groups address the need for LGBTQ+ patient-physician allyship
Universal health care is a core value and a major source of pride amongst Canadians. Canada’s medical institutions are expected to meet the needs of a diverse population, yet the conversation around understanding and delivering quality care to meet trans-specific health needs is full of holes, if not entirely absent.
At the end of February, a panel of experts convened at McGill to discuss the ways public health systems perpetuate outdated practices and institutionalized discrimination against LGBTQ+ people. Healthy McGill and the Nursing Peer Mentorship Program facilitated this safe space and invited audience members to bring the potentially offensive, random, or menial questions they might otherwise be afraid to ask about queer and trans health.
Simple things like asking a patient’s pronouns and prefacing potentially sensitive questions can make a huge and lasting difference, said Wong. The willingness of health care workers to learn and use LGBTQ+ friendly language signifies allyship, which is crucial in building the trust needed to give and receive quality care.
For many of the future health care providers in the room, it was their first opportunity to address health care in an LGBTQ+ context with experts working in the field. For others, it was a chance to gain a better understanding of the barriers trans people face when seeking health care in Montreal and beyond.
In A (Not So) Short Introduction to LGBTQIA2S+ Language, bioethicist and trans activist Florence Ashley defines transgender, often shortened to “trans” as, “a person whose gender identity differs from the gender they were assigned at birth.” They point out, “being trans is independent of one’s choice to take hormones or undergo surgeries.” It is not a sexual orientation, nor is it premised on anatomical criteria.
“For health care providers there’s often the confusion between sex (assigned at birth) and gender,” said panelist Kimberly Wong, a youth sexual health educator at AIDS Community Care Montreal. “When we’re talking about sex, we’re really talking about anatomy. Gender is really a self-feeling kind of thing.”
Health care providers often conflate the two, resulting in the frustrating experience of being repeatedly misgendered, interrogated about one’s transition, or forced to bear the burden of educating the physician about transgender realities in general. A strained patient-physician relationship can inhibit one’s willingness to disclose pertinent medical information, or lead to broad assumptions premised on misinformation. “As soon as you start assuming, things go wrong really quickly. So many people end up with substandard care,” said Ashley.
Simple things like asking a patient’s pronouns and prefacing potentially sensitive questions can make a huge and lasting difference, said Wong. The willingness of health care workers to learn and use LGBTQ+ friendly language signifies allyship, which is crucial in building the trust needed to give and receive quality care.
The process of unlearning outdated terms and practices written into medical literature is still in its early stages, and in the meantime trans people have had to seek out resources and services elsewhere. “Trans people are often very good advocates for themselves because they have to be,” said Eve Finley, an equity facilitator at McGill. “That often translates into these very interesting networks of knowledge sharing that happen online and in person.”
The Centre for Gender Advocacy (CGA), based out of Concordia, is one such network for trans people in Montreal. “A lot of people reach out to us or to other trans organizations and we provide them with such important information,” said D.T., trans advocate and public educator at the CGA. “The role of the center is to provide guidance and resources to people, whether Concordia students or not.”
“Change comes from people advocating for their rights to exist,” said D.T. “That advocacy creates the pressure that cannot be repressed, and it leads to change in policy.”
In collaboration with Concordia Health Services, the CGA reached out to experts in trans health care and organized the opportunity for health services staff to receive training in trans-affirmative care. Concordia is the only university in Quebec to have done so, said D.T, “and they also use the latest approaches to transitioning, namely the informed consent model, where we accompany the person (throughout the process) and validate and affirm their decisions regarding their own body and self.”
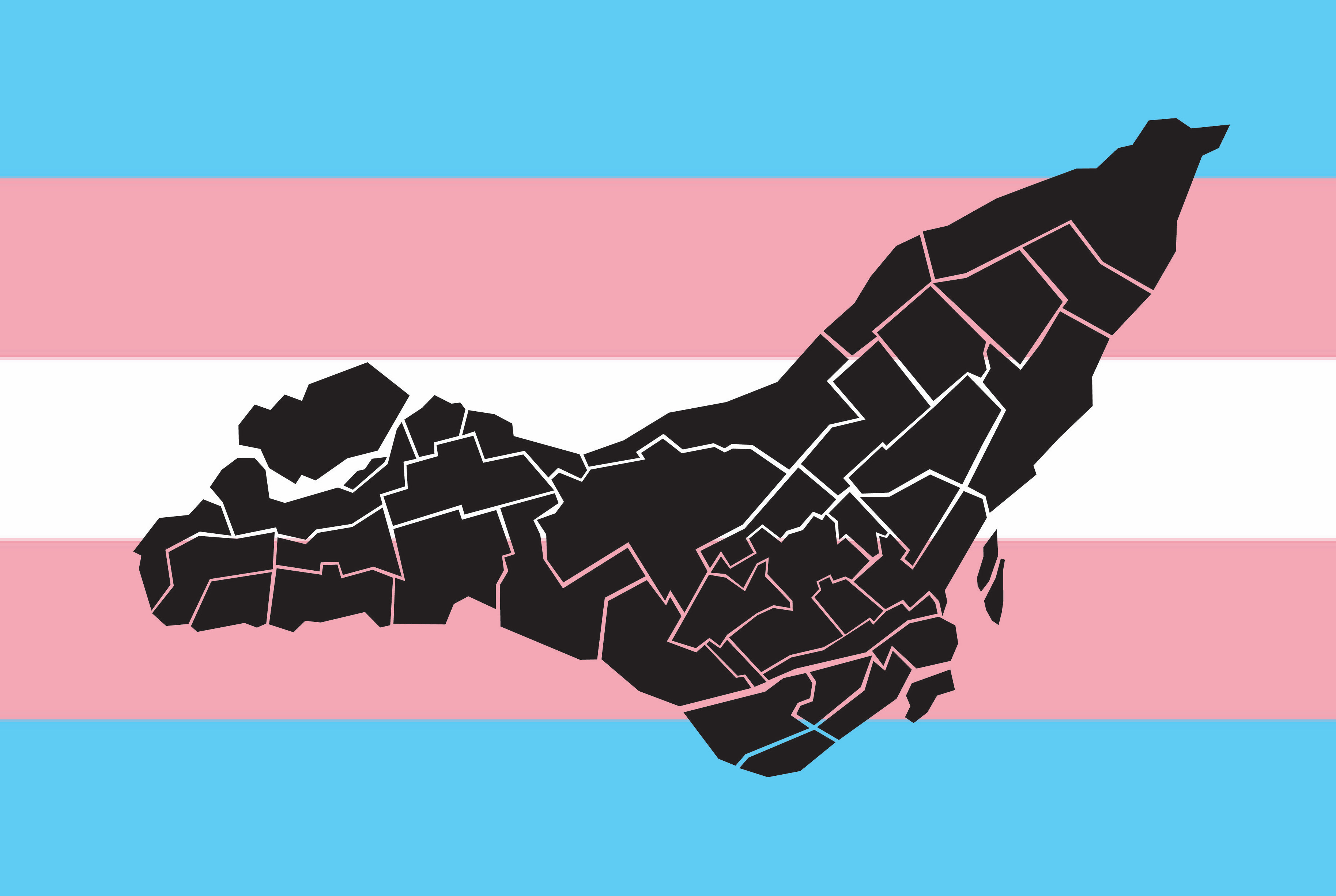
Despite the progress made at Concordia, the public system in Montreal is still rife with hostile spaces and ill-informed doctors unable or unwilling to provide trans-competent care. “Outside Concordia, it’s hit or miss.” said D.T. “If you don’t know who the trans-friendly doctors are, you might end up in the wrong place with someone who will not help you affirm your gender and would rather discourage you from being who you are, which is sad in 2019.” To help avoid these pitfalls, the CGA provides an interactive map of health care providers who have denied services to patients on the basis of their trans identities.
“It’s really difficult to find non-judgemental health providers,” said Wong. “There are so many situations where people will not talk to their doctors or seek care because they fear judgement.” When they do, the reported medical problems are often minimized, dismissed, or blamed on unrelated factors. D.T. called it “trans broken arm syndrome,” which refers to the tendency of health care professionals to blame medical problems that someone might have on their trans status. “It still happens a lot, and many trans people choose not to go to the hospital,” said D.T.
The syndrome is not an isolated phenomena, and it’s one with significant repercussions. A 2012 study of trans people’s medical experiences in Ontario found that over half of respondents had negative experiences in clinical settings, and 21 per cent opted not to seek emergency care due to fear of being mistreated. The Twitter hashtag #transhealthfail is an online repository for first-person accounts of such encounters, offering a glimpse at incidents ranging from careless misgendering to outright denials of service from health care providers.
With so few capable physicians in the Montreal area, even those who do manage to seek them out end up waiting weeks or months for an appointment. “We know from research and from people’s personal experiences [that] that time between discovering, affirming to yourself that you are trans and starting transitioning is the time when people go through the most distress,” added D.T. “The longer they wait, the longer they experience dysphoria.”
While the gains made at Concordia signify positive change, D.T said there is still a long way to go to reach a trans-affirmative standard of care in Montreal and beyond. “We know very well that the trans health care field evolves very quickly. There are new needs, new approaches, and so the trainings [Concordia Health Services] did should be ongoing.”
A belief in universal health care is a belief in offering accessible care to meet the unique health needs of all Canadians, and trans-affirmative care is no exception. Of all the things that can be done to improve the quality of services for trans people on a local level, D.T. said it starts with education and advocacy. “Change comes from people advocating for their rights to exist. That advocacy creates the pressure that cannot be repressed, and it leads to change in policy.”
Feature graphic by Mackenzie Lad
Article updated on Jan. 31. 2024 – One of the sources of this article has come forth and requested to be anonymous.